|
|
 |
|
| 1997 |
|
 Last
Acts' Innovations
in End-of-Life Care: An International Journal and
On-line Forum for Leaders in End-of-Life Care.
This is an online journal published by the Center for
Applied Ethics and Professional Practice (CAEPP) at the Education Development Center (EDC) in Newton, Massachusetts
(Mildred Solomon). Last
Acts' Innovations
in End-of-Life Care: An International Journal and
On-line Forum for Leaders in End-of-Life Care.
This is an online journal published by the Center for
Applied Ethics and Professional Practice (CAEPP) at the Education Development Center (EDC) in Newton, Massachusetts
(Mildred Solomon).
|
| 1997 |
|
 Promoting
Excellence in End-of-Life Care (RWJF): $12 million+ from
RWJF to Ira Byock and his institute based at the Univ.
of Montana - Missoula. Promoting
Excellence in End-of-Life Care (RWJF): $12 million+ from
RWJF to Ira Byock and his institute based at the Univ.
of Montana - Missoula. |
| 1997 |
Jan |
Dorgan (D-ND) and Ashcroft (R-MO) begin seeking support
for proposed legislation to prevent federal funding
of PAS. The legislation was titled "Assisted Suicide
Funding Restriction Act of 1997" (S. 304; companion
bill to HR 1003). |
| 1997 |
Feb |
Oregon:
On February 27, the Ninth Circuit Court of Appeals dismisses the district court's decision, claiming the federal
court did not have jurisdiction:
"The plaintiffs in this case
are doctors, patients, and residential care facilities
challenging the facial validity of the State of Oregon's
Death With Dignity Act. Plaintiffs contend the Act
violates the First and Fourteenth Amendments to the
United States Constitution, as well as several federal
statutes. The district court found the Act to violate
the Equal Protection Clause and permanently enjoined
its enforcement. Because the federal courts do not
have jurisdiction to entertain Plaintiffs' claims,
we vacate and remand with instructions to dismiss
Plaintiffs' complaint."
|
| 1997 |
Mar |
Hastings Center Report publishes "Is
There a Duty to Die?" by John Hardwig. (Mar-Apr;27(2):34-42.)
Hardwig answers "yes," for the common good.
"Let me be clear. I certainly
believe that there is a duty to refuse life-prolonging
medical treatment and also a duty to complete advance
directives refusing life-prolonging treatment. But
a duty to die can go well beyond that. There can be
a duty to die before one's illnesses would cause death,
even if treated only with palliative measures. In
fact, there may be a fairly common responsibility
to end one's life in the absence of any terminal illness
at all. Finally, there can be a duty to die when one
would prefer to live. Granted, many of the conditions
that can generate a duty to die also seriously undermine
the quality of life. Some prefer not to live under
such conditions. But even those who want to live can
face a duty to die."
|
| 1997 |
Apr |
 RWJF
funds a television broadcast: Before
I Die, hosted by Tim Russert. The program
airs on PBS on April 22. This begins the media campaign
that will build grass roots organizations, purportedly
as a reaction to the SUPPORT study. Funding: $639,000
from RWJF to Educational Broadcasting Corp; $181,000
to Barksdale Ballard for public relations. RWJF
funds a television broadcast: Before
I Die, hosted by Tim Russert. The program
airs on PBS on April 22. This begins the media campaign
that will build grass roots organizations, purportedly
as a reaction to the SUPPORT study. Funding: $639,000
from RWJF to Educational Broadcasting Corp; $181,000
to Barksdale Ballard for public relations.
|
| 1997 |
Apr |
The Assisted
Suicide Funding Restriction Act (H.R.
1003) approved by the House on 4/10, and passed the
Senate on 4/16. Signed by President Clinton on 4/30. |
| 1997 |
May |
Schiavo: George
Felos (a founding member of the National Legal Advisors
Committee on Choice in Dying) is brought into the case
"[Michael Schiavo] is aware that the issue of withdrawal
or refusal of medical treatment for [Terri Schiavo]
is a difficult issue in this case and that the ward's
parents will need to be involved. I am not aware
of any other interested persons. Because of
the delicate nature of this case, I advised [Michael]
to employ counsel who has special expertise in this
area of the law.
It is anticipated that the parents will initially
be approached gently and informally by Attorney Felos
regarding this issue, that Hospice will be involved,
and that counseling will be provided to the guardian
and the parents to assist with the decision-making
process." [Bushnell
letter, 5/6/97]
|
| 1997 |
May |
 The Pain & Policy Studies
Group at the Univ. of Wisconsin-Madison receives
$693,400 from RWJF (#31461) to work "with state
medical, nursing, and pharmacy boards to help them
make more informed decisions with regard to physician
practice in the treatment of pain, and collected data
on pain-related policy and practice." This is the project
that resulted in North
Carolina's "Joint Statement on Pain Management
in End-of-Life Care." The Pain & Policy Studies
Group at the Univ. of Wisconsin-Madison receives
$693,400 from RWJF (#31461) to work "with state
medical, nursing, and pharmacy boards to help them
make more informed decisions with regard to physician
practice in the treatment of pain, and collected data
on pain-related policy and practice." This is the project
that resulted in North
Carolina's "Joint Statement on Pain Management
in End-of-Life Care."
|
| 1997 |
May |
 Soros
and RWJF co-sponsor the "National Consensus Conference
on Medical Education for Care Near the End of Life,"
held May 16-17 in Washington, DC. RWJF granted
$41,500 to Harvard Pilgrim Healthcare, Inc, and Susan
Block, MD (Director, PDIA Faculty Scholars program);
David Barnard, PhD, was co-chair. The conference produced
a consensus statement, endorsed by the following people: Soros
and RWJF co-sponsor the "National Consensus Conference
on Medical Education for Care Near the End of Life,"
held May 16-17 in Washington, DC. RWJF granted
$41,500 to Harvard Pilgrim Healthcare, Inc, and Susan
Block, MD (Director, PDIA Faculty Scholars program);
David Barnard, PhD, was co-chair. The conference produced
a consensus statement, endorsed by the following people:
Judith
Ahronheim, M.D (Soros/PDIA Faculty
Scholar 1995);
Robert Arnold,
M.D. (a founding member of Society for Health
& Human Values);
J. Andrew Billings,
M.D. (Soros/PDIA Faculty Scholar 1995);
Harvey Max Chochinov (Canada; Soros/PDIA 1996)
Stuart Farber,
M.D. (Soros/PDIA Faculty Scholars 1995);
Frank Ferris, M.D.
(Soros/PDIA Faculty Scholar);
Marilyn Field,
Ph.D. (IOM);
Joseph Fins, M.D. (Soros/PDIA Faculty Scholar 1997); |
Kathleen
Foley, M.D. (Director, Soros/PDIA)
Ellen Fox, M.D.
Jack Gordon (Last
Acts Institution Innovation committee; Hospice Foundation
of America is Soros grantee)
Barbara Koenig,
Ph.D. (Soros/PDIA 1999);
Karen Long;
Edward Lowenstein,
M.D.;
Diane Meier, M.D. (Soros/PDIA Faculty Scholar 1995);
Galen Miller (National Hospice Organization);
Patricia Prem,
M.S.W. (Founder, Project on Death in America);
|
Christina
Puchalski, M.D. (Convener of Last Acts Spirituality
Task Force);
Timothy Quill,
M.D.
Fenella
Rouse, J.D. (1998 Kornfeld executive director);
Colleen Scanlon,
R.N., J.D., MS;
Peter Selwyn, M.D.,
M.P.H. (Soros/PDIA Faculty Scholar 1997);
Mildred Solomon,
Ed.D.;
R. Knight Steel,
M.D.;
Wayne Ury, M.D.;
Charles von Gunten, M.D., PhD (Soros/PDIA
1995);
David Weissman,
M.D.; (Soros/PDIA 1995);
Stuart Youngner,
M.D. |
|
| 1997 |
Jun |
Publication of IOM's book, "Approaching
Death." The report included futility guidelines,
and a recommended strategy for changing the culture.
RWJF adopted the strategy in their end-of-life project
funding strategy:
- Professional Education;
- Institutional
change;
- Public engagement.
|
| 1997 |
Jun |
June
25, the board of the American Academy of Hospice and Palliative
Medicine (AAHPM)
adopts a position
statement on assisted-suicide, taking a neutral position,
but offering rough guidelines in case PAS is legalized. |
| 1997 |
|
US Supreme Court cases:
On June 26, the US Supreme Court reversed two
Circuit Court decisions. The Supreme Court
decisions helped map out a strategy for the Last
Acts' new and improved definition of assisted
suicide. Four years after the decisions,
Last Acts' Karen Orloff Kaplan and Margaret Metzger
wrote:
"In these cases, the Supreme Court upheld the
right of states to legislate whether to ban
or to permit assisted suicide. The Supreme
Court concluded that the distinctions between
assisted-suicide and either withholding or withdrawing
life-sustaining treatment were "important,"
"logical," and "rational." As a result,
it is constitutionally permitted for states
to allow competent persons to refuse life-sustaining
treatments while banning physician-assisted
suicide. Amidst all of the publicity about
the activities of Dr. Jack Kevorkian, Oregon
became the only state to legally permit, in
limited circumstances, physician-assisted suicide."*
Karen Kaplan's right-to-die group,
Choice in Dying, posted a summary
of the decisions.
Hemlock
Society founder Derek Humphry notes that the
Supreme Court "also validated the concept of 'double
effect,' openly acknowledging that death hastened
by increased palliative measures does not constitute
prohibited conduct so long as the intent is relief
of pain and suffering."
Professor Russell
Hittinger's incisive article in the March,
1997, issue of First
Things parses the Clinton administration's
amicus curiae briefs, and anticipates a decision
that would nominally oppose assisted suicide,
while at the same time open the door to assisted
suicide on a state-by-state basis.
*Metzger
JD, M., Kaplan MPH, Sc.D., Karen (2001). Transforming
death in America: A state of the nation report.
Washington, DC. Prepared for Last Acts.
|
|
| 1997 |
Aug |
 RWJF announces a three-year, $1.6 million grant to the University of
Wisconsin - Madison Medical School. "Under this
project, the Wisconsin Cancer Pain Initiative--a national
leader in encouraging better methods of pain control and
in teaching health care professionals how to use them--will
work with the [Joint Commission on Accreditation
of Healthcare Organization (JCAHO)]
to develop new pain control standards."
[full text of press release ] RWJF announces a three-year, $1.6 million grant to the University of
Wisconsin - Madison Medical School. "Under this
project, the Wisconsin Cancer Pain Initiative--a national
leader in encouraging better methods of pain control and
in teaching health care professionals how to use them--will
work with the [Joint Commission on Accreditation
of Healthcare Organization (JCAHO)]
to develop new pain control standards."
[full text of press release ] |
| 1997 |
Sep |
National Institutes
of Health responds to SUPPORT with a Research Workshop
on September 2 titled "Symptoms in Terminal Illness." |
| 1997 |
Sep |
 RWJF
grant for $149,486 (ID#32334) to National
Conference of State Legislators for a study of
state legislation, that would lead to publication of
a book for legislators, to guide them in crafting end-of-life
legislation. RWJF
grant for $149,486 (ID#32334) to National
Conference of State Legislators for a study of
state legislation, that would lead to publication of
a book for legislators, to guide them in crafting end-of-life
legislation.
"Working with the Center
to Improve Care of the Dying at George Washington
University, the National Conference of State Legislatures
(NCSL) produced and distributed 10,500 copies of the
guidebook State Initiatives in End-of-Life Care: Policy
Guide for State Legislatures. The guidebook describes
state commissions examining End-of-Life issues, explores
pain management, and discusses financing of services
for the terminally ill. NCSL also held seminars featuring
legislators and End-of-Life experts at two of its
national conferences. In addition, the organization
produced and distributed 2,500 copies of two audiotapes
— "State Initiatives in End-of-Life Care" —
based on these seminars. Educational materials were
provided at no cost to state legislators and their
staffs"
First conference, State Initiatives on End-of-Life
Care, in December 1997 Panelists: George Eighmey (Ex. Director of Compassion in
Dying, Oregon); Joan Gibson, M.D.; Peter Ginaitt; David
Joranson, M.S.S.W.; Susan Lynch; Joanne Lynn, M.D.,
MA, MS.
Concurrent RWJF funding to Richard Merritt at NCSL,
and to GWU, for state-level health policy:
1995 ID #20033 George Washington University $253,126
1996 ID #30342 National Conference of State Legislatures
$303,120
1997 ID #31569 National Conference of State Legislatures
$702,120
1999 ID #35554 National Conference of State Legislatures
$229,684
1999 ID #37549 National Conference of State Legislatures
$233,436
The manual to assist state legislators would be published
in June, 1998 (see below) |
| 1997 |
Oct |
American Health Decisions
(AHD) (Atlanta, GA, and Appleton, WI; with
"grass roots" groups in 13 states) produces The
Quest to Die With Dignity (online executive
summary).
AHD received a grant of $254,000 from RWJF to conduct
the study. Based on 385 people in 32 focus groups, and
29 additional telephone conversations, AHD determined
that Americans "fear dying while hooked up to machines,"
and spells out how "ethnic background [more than religion]
accounts for the greatest differences" in "opinions,
values, and concerns."
AHD had planned to release
the report in July, "at an opportune time to benefit
two other initiatives:" EPEC, and "a national
education program that will parallel the AMA's program"
[Last Acts]. The report was released in early
October, in time to be featured in the Oct. 29 Last
Acts conference (see below).
|
| 1997 |
Oct |
October 29-30: Last
Acts, Second
National Leadership Conference. Over 275 attendees.
Welcome via videotape from Honorary Chair Rosalynn Carter.
Ira Byock gave keynote address on "finding
the levers to move a culture of denial" in America."
Byock identified:
Levers
of Change:
1) Standards
2) Measurement based on standards.
3) Accreditation and Certification
4) Policy and Public |
Agents
of Change:
1) Medical Establishment
2) Boomer Consumers
3) Payers
4) Funders of Research and Demonstrations
5) Media
|
|
| 1997 |
Oct |
Oregon's
Death With Dignity Act (ORS 127.800-897) takes effect
October 6 when the U.S. Supreme Court dismisses a writ
of certiorari |
| 1997 |
Dec |
December 9: Alliance
for Health Reform, Choice in Dying, and Hospice Organization
of America co-sponsor congressional
briefing on the Advance Planning and Compassionate
Care Act of 1997. The bill was sponsored by Sen.
Jay Rockefeller and Sen. Susan Collins, and was "designed
to strengthen the Patient Self-Determination Act." |
| 1997 |
|
 Precepts
of Palliative Care (Last Acts Palliative
Care Committee) Precepts
of Palliative Care (Last Acts Palliative
Care Committee)
Last Acts says the document "Describes the essential components
of palliative care. Prepared by the Last Acts Palliative
Care Task Force, headed by Colleen Scanlon (Catholic
Health Initiatives) and Karen Lomax (National Center
for Clinical Ethics, US Department of Veterans Affairs),
the precepts have been accepted by more than 25 national
and 35 state and local organizations. They provide a
basis for discussion of what constitutes good end-of-life
care in any clinical setting. They are being used by
hospitals, hospices, and professional training programs."
The Palliative Care Task Force included:
- Colleen Scanlon, R.N., J.D., MS--Catholic Health
Initiatives (Denver, CO)--Convener
- J. Andrew Billings, M.D.-- Massachusetts General
Hospital; Soros/PDIA Faculty Scholar 1995;
- Ira Byock, M.D.-- Missoula Demonstration Project;
- Margaret Campbell, R.N., M.S.N.-- American Association
of Critical Care Nurses;
- Charles Cleeland, Ph.D.-- American Pain Society
(M.D. Anderson Cancer Center);
- Marilyn Field, Ph.D.--Institute of Medicine;
- Russell Portenoy, M.D.-- Beth Israel Medical Center,
NYC;
- Fenella Rouse, J.D.--Mayday Fund;
- Bonnie Ryan, R.N.-- Community Based Services, Dept.
of Veteran Affairs;
- Marguerite Stevens, Ph.D.--Dartmouth-Hitchcock Medical
Center;
- H. James Towey --Florida Commission on Aging with
Dignity;
- Connie Zuckerman, J.D.--United Hospital Fund; Hospital
Palliative Care.
|
| 1998 |
|
 Choice in Dying launches coordinating
center for grant money aimed at "Program to Improve the
Selection and Performance of Health Care Agents."
Grant for $115,000
from Samuels Foundation establishes the center.
Samuels provided an additional $290,000 in 2000. Partnership for Caring announced
the appointment of administrator for the center in their Fall,
2000, newsletter. Choice in Dying launches coordinating
center for grant money aimed at "Program to Improve the
Selection and Performance of Health Care Agents."
Grant for $115,000
from Samuels Foundation establishes the center.
Samuels provided an additional $290,000 in 2000. Partnership for Caring announced
the appointment of administrator for the center in their Fall,
2000, newsletter. |
| 1998 |
|
 First
steps to Partnership for Caring: An early 1998 “historic meeting of leaders in
the end-of-life field” is impetus for updating
the organization, from Choice in Dying to "Partnership
for Caring." Karen Kaplan and Ira Byock wrote in the
Winter, 1998, Choice in Dying newsletter that Partnership
for Caring will be a grass-roots, consumer-driven, activist
organization that will "put significant pressure on
federal and state governments." First on board was AAHPM.
The authors continue (emphasis added): First
steps to Partnership for Caring: An early 1998 “historic meeting of leaders in
the end-of-life field” is impetus for updating
the organization, from Choice in Dying to "Partnership
for Caring." Karen Kaplan and Ira Byock wrote in the
Winter, 1998, Choice in Dying newsletter that Partnership
for Caring will be a grass-roots, consumer-driven, activist
organization that will "put significant pressure on
federal and state governments." First on board was AAHPM.
The authors continue (emphasis added):
“Response to the formation
of Partnership for Caring has been very enthusiastic.
First to join were Choice In Dying and the American Academy of Hospice and Palliative Medicine [AAHPM]. The Boards of Directors of
both Choice In Dying and the Academy
voted unanimously to join Partnership for Caring as
collaborating organizations. Choice In Dying will
offer its members complimentary one-year memberships
in Partnership for Caring. Other organizations such
as the Older Women's League, National Academy
of Elder Law Attorneys, and the Commission
on Legal Problems of the Elderly, have also agreed
to participate in Partnership for Caring.”
|
| 1998 |
Jan |
 $216,600
from RWJF to Univ. of California-San Francisco,
for medical textbook revision study.
Conducted by Last Acts Provider Education Task Force. $216,600
from RWJF to Univ. of California-San Francisco,
for medical textbook revision study.
Conducted by Last Acts Provider Education Task Force.
Co-Conveners of the task force: Stephen McPhee, Anne
Rhome. Textbook study headed by J. Andrew Billings*
and Steven Pantilat.**
Other task force members included: Robert
Arnold, Susan Blacker, Susan Block*, Grace Christ*,
Deborah Danoff, Betty Ferrell*, Ellen Fox, James Hallenbeck,
Thomas Prendergast*, Michael Rabow**, Kelley Skeff,
Charles von Gunten*, David Weissman.*
*1995-97 Soros/Project
on Death in America grant recipients.
** Soros/PDIA grant recipients after 1998. |
| 1998 |
Mar |
Under the guidance of
the Center for Ethics in Health Care at Oregon Health
& Science University, the Task Force to Improve the
Care of Terminally Ill Oregonians produced Oregon
Death With Dignity Act: A
Guidebook for Health Care Providers. In the guidebook, PAS
is comfort care. Principals included:
Patrick Dunn, M.D., Task Force Chair; Bonnie Reagan, M.D.,
R.N., Editor; Susan Tolle, M.D.,
Reviewer and Major Contributor; Elizabeth Mitchell, M.S.W.,
L.C.S.W., Project Administrator; Ann Jackson, MBA (Oregon
Hospice Assn); Linda Ganzini, MD (Soros/PDIA 1998).
(Funded by Greenwall Foundation) |
| 1998 |
Apr |
 Pain
control: First step toward Bergman
v. Chin: Beverly Bergman, with the assistance of Compassion
in Dying, files a complaint at the Medical Board
of California against Dr. Wing Chin. Ms. Bergman
charged that Dr. Chin had under-prescribed pain medication
for her terminally ill father. In June, 2001, an
Alameda County jury awarded Bergman's family $1.5 in damages.
The final judgment and settlement came a year later, in June, 2002 (see below).
Compassion in Dying's legal assistance in this case was
financed in part by a $60,000 contribution from the Mayday
Fund. Pain
control: First step toward Bergman
v. Chin: Beverly Bergman, with the assistance of Compassion
in Dying, files a complaint at the Medical Board
of California against Dr. Wing Chin. Ms. Bergman
charged that Dr. Chin had under-prescribed pain medication
for her terminally ill father. In June, 2001, an
Alameda County jury awarded Bergman's family $1.5 in damages.
The final judgment and settlement came a year later, in June, 2002 (see below).
Compassion in Dying's legal assistance in this case was
financed in part by a $60,000 contribution from the Mayday
Fund. |
| 1998 |
Apr |
Christine
Cassel, Diane Meier, Sean Morrison, Timothy Quill produce
a "Survey of Physician Assisted Suicide and Euthanasia
in the United States" (NEJM, 4/23/98). The next day, the New York Times publishes Diane Meier's "Change of Heart" on assisted
suicide. |
| 1998 |
Jun |
 Community-State
Partnerships to Improve End of Life (C-SP). [Note: This item was originally listed on the timeline
in "January, 1999," because that was when funding was
announced and state partnerships began forming. We've
moved the item to 1998 to reflect the earlier planning.] Community-State
Partnerships to Improve End of Life (C-SP). [Note: This item was originally listed on the timeline
in "January, 1999," because that was when funding was
announced and state partnerships began forming. We've
moved the item to 1998 to reflect the earlier planning.]
Community-State Partnerships was an
$11.5 million project directed by the Midwest Bioethics
Center. Planning began in 1998; the first grants would
not be awarded until January, 1999.
Designed to bring about change at the
state and local levels, C-SP used Oregon Health Decisions
(OHD) as a model. C-SP devoted the first few policy
briefs — particularly June and October, 1998
— to discussion of Michael Garland, Ralph Crawshaw,
and the OHD experiment. Successes included an increase
in the number of DNRs signed, and healthcare rationing.
The June issue reported that OHD assesses community
values, then “tries to stimulate local democracy
by seeking out local leaders and tapping into existing
networks with ready-made constituencies like Oregon’s
Hospice Association or the local Rotary Club. 'Anywhere
where there are enclaves with a feeling of community,'
says Crawshaw.”
OHD provided the roadmap in 1998, but
RWJF also credited James Towey's Aging with Dignity.
An RWJF
grant report notes that Towey "helped shape a new
[Robert Wood Johnson] Foundation national program, Community-State
Partnerships to Improve End-of-Life Care, which supports
organizations working to stimulate community dialogue
and improve the quality of End-of-Life care."
Myra Christopher, president of Midwest
Bioethics Center, would also credit bioethics centers
and networks of hospital ethics committees for development
of the state-level coalitions. This was the focus of
her article for Pain Medicine, titled "Role
of Ethics Communities, Ethics Networks, and Ethics Centers."
A prime example of the way in which bioethics groups
created a network of influence at the state level can
be seen in the case study of the Florida Partnership
[see "The Florida Experiment"].
In January, 1999, RWJF announced the
first round of C-SP grants. By 2001, C-SP would form
End-of-Life Partnerships and coalitions in 21
states:
Alabama, California, Connecticut, DC, Florida, Hawaii,
Iowa, Kansas, Kentucky, Maine, Michigan, Minnesota,
Nevada, New Hampshire, New Jersey, North Carolina, North
Dakota, Oklahoma, Rhode Island, Utah, West Virginia.
Susan Tolle, MD, director of
Oregon Health & Science University's Center for
Ethics in Health Care, was chair of C-SP's National
Advisory Committee. Tolle is quoted in the first
policy brief:
“Our use of data with
the news media often precedes efforts to bring about
change in other settings. . . . If data have
not been presented effectively to a wider audience,
we are unlikely to be of tremendous influence to legislative
bodies. And don't forget that physicians read newspapers.
There is no doubt that The
Oregonian has made a huge difference.
You can help change the culture of medicine through
the popular press. Now the question is, how can we
make the climate receptive to the next wave of changes?”
[Issue
1; June 1998 (PDF)]
One of CSP's first projects was coordinating
groups for Bill Moyers' PBS special, On Our Own Terms. For example, Midwest Bioethics Center's president
Myra Christopher traveled to Florida
in October, 1999, to coordinate activists from across
the country for the program [see
2000]. The Moyers project would later blossom into "Rallying
Points" led by Karen Kaplan of Partnership
for Caring [see January,
2001].
Community-State Partnerships coordinated
their work with the University of Wisconsin-Madison's Pain
& Policies Study Group (PPSG) (a World
Health Organization collaborating agency) program to
reform regulations of controlled substances at the state
level across the US. PPSG targeted 16 states for
reform, all of which had C-SP coalitions (CA,
CT, HI, IA, KS, KY, ME, NV, NC, NY, ND, OK, RI, TX,
UT, and WV.)
The C-SP program ended in 2003. C-SP
policy brief 19 (June, 2003) provides a state-by-state
list of goals and coalition accomplishments.
In May, 2004, Midwest Bioethics Center announced they
had changed their name to Center
for Practical Bioethics. The policy briefs
continue at the new
site.
[Policy Brief #22 contains the usual misinformation
about the Terri Schiavo case. Brief #24 discusses protecting
the right-to-die for minorities and disabled. Hugh Gallagher
is quoted, but not identified as a Compassion in Dying
board member who argued in favor of PAS. Gallagher's
organization, "Autonomy," was founded with the help
of a grant to Compassion in Dying from the Gerbode Foundation.]
[Next: see On Our Own Terms (Sep.
2000), then Rallying
Points (Feb. 2002)] |
| 1998 |
Jun |
 Manual
published: "State Initiatives in End-of-Life Care Policy
Guide for State Legislators" (funded by RWJF) Manual
published: "State Initiatives in End-of-Life Care Policy
Guide for State Legislators" (funded by RWJF) |
| 1998 |
Oct |
October 1: Hugh Finn's
feeding tube is removed.
(Case goes to Virginia Supreme Court)
Hugh Finn was a high-profile
figure in Louisville, Kentucky, where he had been
news anchor. In 1995 he was left brain-damaged
after an auto accident. He was moved to
Virginia for rehabilitation. In June, 1998,
his wife Michele requested that his feeding tube
be removed. On August 31 Circuit Court Judge
Frank A. Hoss ordered the removal. Finn's
parents and siblings, and his nurse, contended
Finn was not in a PVS, and had spoken to them
repeatedly. The family sought help from Robert
Marshall, a delegate in Virginia's House.
Judge Hoss ordered that the feeding tube be removed
on October 1. Virginia governor James Gilmore
appealed to the Virginia Supreme Court, but his
appeal was rejected almost immediately.
Hugh Finn died on October 8, 1998.
The Virginia
Supreme Court revisited the case in 2000,
when Michele Finn sued the state for reimbursement
of legal expenses. This time the court decided
in favor of the governor, and ruled that the governor's
1998 intervention had been warranted.
Robert
Marshall's web site is an excellent resource
for facts in the case.
|
|
| 1998 |
Oct |
October 2: John
Paul II addresses the bishops of California, Nevada,
and Hawaii on their "ad Limina" visit. He states:
"As ecumenical witness in defense of life develops,
a great teaching effort is needed to clarify the substantive
moral difference between discontinuing medical procedures
that may be burdensome, dangerous or disproportionate
to the expected outcome - what the Catechism
of the Catholic Church calls “the refusal
of 'over-zealous' treatment” (No. 2278; cf. Evangelium
Vitae, 65) - and taking away the ordinary means
of preserving life, such as feeding, hydration and
normal medical care. The statement of the United States
Bishops' Pro-Life Committee, Nutrition and Hydration:
Moral and Pastoral Considerations, rightly emphasizes
that the omission of nutrition and hydration intended
to cause a patient's death must be rejected and that,
while giving careful consideration to all the factors
involved, the presumption should be in favor of providing
medically assisted nutrition and hydration to all
patients who need them. To blur this distinction is
to introduce a source of countless injustices and
much additional anguish, affecting both those already
suffering from ill health or the deterioration which
comes with age, and their loved ones."
|
| 1998 |
Oct |
 Veterans
Affairs Faculty Program (EPEC for veterans). First
Leadership Conference is held in Warrenton, Virginia.
Report for the RWJF
grant ($982,000). VA Faculty steering committee included:
Christine Cassel; Timothy Quill; James Hallenbeck; Kelley
Skeff; James Tulsky. Among the first VA Faculty Leaders
were David Casarett, David Lowenthal, Thomas Prendergast
(Soros/PDIA), and James Cleary (Soros/PDIA). Veterans
Affairs Faculty Program (EPEC for veterans). First
Leadership Conference is held in Warrenton, Virginia.
Report for the RWJF
grant ($982,000). VA Faculty steering committee included:
Christine Cassel; Timothy Quill; James Hallenbeck; Kelley
Skeff; James Tulsky. Among the first VA Faculty Leaders
were David Casarett, David Lowenthal, Thomas Prendergast
(Soros/PDIA), and James Cleary (Soros/PDIA). |
| 1998 |
Nov |
Hastings Center's Humans and Nature Project hosts the first meeting with the International Union for Conservation of Nature (IUCN), a step toward drafting the Earth Charter. Three more meetings would follow, rotating between the Hastings Center and the Pocantico Center.
Four years later, in 2002, the Humans and Nature Project would spin off to become the Center for Humans and Nature, with Strachan Donnelly as president. Bruce Jennings would join Donnelly in directing the new organization. (Jennings is best known for his work in medical ethics. In 1987 he was associate project director of the Center's important Guidelines on the Termination of Life-Sustaining Treatment and the Care of the Dying, and in 2007 advised the 3-year project to update the Guidelines on Termination of Life-Sustaining Treatment.)
|
| 1998 |
Dec |
 Financed
by a $39,900 grant from RWJF in 1997, the Radio
and Television News Directors Foundation was
able to "research, write, produce and disseminate The
Journalist's Resource Guide on End-of-Life Issues."
Eric Swanson, executive director of RTNDA at the time,
was named project director for the grant. (Swanson became
chief operating officer of Common Cause several years
later.) In December, 1998, RTNDF produced the
guide: Covering
the Issues of Death and Dying. Financed
by a $39,900 grant from RWJF in 1997, the Radio
and Television News Directors Foundation was
able to "research, write, produce and disseminate The
Journalist's Resource Guide on End-of-Life Issues."
Eric Swanson, executive director of RTNDA at the time,
was named project director for the grant. (Swanson became
chief operating officer of Common Cause several years
later.) In December, 1998, RTNDF produced the
guide: Covering
the Issues of Death and Dying.
The guide misinforms on several important
court cases. For example, following is a summary
of the Cruzan case. It confuses "feeding
tubes" with "machines," and neglects the fact that hearsay
evidence was used by the lower court to determine Nancy
Cruzan's supposed wishes:
"1990 – The U.S. Supreme
Court rules against Nancy Cruzan’s parents,
who wanted to disconnect life-support systems from
their daughter, an accident victim living in a persistent
vegetative state. The High Court rules there was insufficient
evidence that Nancy Cruzan would have wanted life-sustaining equipment removed, and sends the case back to the State of Missouri.
Missouri state courts—after hearing more witnesses
provided by the Cruzans—allow her to be taken
off feeding
tubes. After the machines are removed, Cruzan dies."
With regard to the Quinlan case, the
authors sought the expert opinion of T. Patrick Hill
of Park Ridge Center in Chicago (pg. 18). The
guide does not disclose that Mr. Hill had been director
of education for Choice in Dying, and advocated euthanasia
in limited circumstances (ref: International
Task Force FAQ, Q. #14).
Choice in Dying is cited throughout
the manual, and is described as "well known for creating
the first living will in 1967." There is no mention
that at that time -- 1967-- the organization was overtly
pro-euthanasia. (For a critical review of living
wills, see: N. Valko, "Of
Living Wills and Butterfly Ballots")
The guide not only recommends Choice
in Dying as a source, but there's a call to action when
it offers a "Story Idea:"
"What is your state’s
law regarding advance directives? Are there
any changes in the works? How many people use advance
directives? Choice in Dying (202/338-9790) can provide
a state-by-state breakdown of laws governing living
wills and the appointment of health care agents. Is
there anything in your state’s law that makes
it easy or difficult for people to express their end-of-life
preferences?"
Meanwhile, Compassion in Dying is described
mildly as an "advocacy group [that] sponsored
the court challenges to New York and Washington state
laws banning physician-assisted suicide." Elsewhere
in the guide, Compassion in Dying is listed as a resource
that "provides counseling, emotional support and information
for terminally ill patients and intensive pain management,
comfort or hospice care, and rational suicide."
|
| 1998 |
Dec |
National
Hospice Outcomes Planning (RWJF)
National Hospice Work Group
(NHWG) and National Hospice Organization (which
becomes NHPCO) launch the planning
phase of what would be a 3-year study of the effectiveness
of hospice care "to create systems and processes that
allow patients to 'die with dignity.' . . . A goal of
the completed project is to create a large, national,
integrated database of what works best, and when, in
managing hospice patients."
NHPCO and NHWG seek the following outcomes:
- Comfortable Dying,
- Safe Dying,
- Self Determined Life Closure [?]
- Effective Grieving.
Studies were conducted at the following sites from
1998-2000:
- Hospice of Winston-Salem (NC)
- Hospice of North Central Florida (Gainesville, FL)
- Hospice of the Bluegrass (Lexington, KY)
- Center for Hospice and Palliative Care (Cheektowaga,
NY)
- Trinity Care Hospice (Torrance, CA)
- Hospice of North Central Ohio (Ashland, OH)
- Hospice of Chatham County (Pittsboro, NC)
- Valley Hospice (Steubenville, OH)
- Hospice of the Piedmont (High Point, NC)
- Hospice of the Florida Suncoast (Largo, FL)
- Hospice of Palm Beach County (West Palm Beach,
FL)
- Hospice of the Western Reserve (Cleveland, OH)
- Hospice of Louisville (Louisville, KY)
- San Diego Hospice (San Diego, CA)
- Hospice of the Valley (San Jose, CA)
- Hospice Care Corporation (Kingwood, WV)
Evaluation Advisory Panel Members:
Carolyn Cassin, M.P.A. (VistaCare); Melanie Merriman,
Ph.D. (formerly with Vitas Healthcare); Peggy Parks,
Ph.D. (Health Care Financing Administration -- Medicare);
Judi Lund Person (Carolinas Center for Hospice and End
of Life Care); True Ryndes, A.N.P., M.P.H. (National
Hospice Work Group); Brad Stuart, M.D. (VNA & Hospice
of Northern California); Joan Teno, M.D., M.S. (Center
for Gerontology and Health Care Research, Brown University);
Diana Wilkie, Ph.D., R.N. (University of Washington
School of Nursing).
Working Group Members (from the hospices):
Kathy Egan, M.A., B.S., R.N. (Hospice Institute of the
Florida Suncoast); Marilyn Follen, M.S.N, R.N. (Proactive
Health Services); Laurel Herbst, M.D. (San Diego
Hospice); Mindy Lawrence, R.N., B.S.N., O.C.N., C.R.N.H.
(Houston Hospice); Susan Mann, B.A., R.N. (Hospice Inc.,
Wichita, KS); Patricia Murphy (VNA & Hospice of
Northern California); Jean Parzuchowski, R.N., M.S.
(Hospice of Michigan); Jean Tilley (Lutheran Hospice,
Irmo, SC);
RWJF funding to National Hospice
and Palliative Care Organization (NHPCO):
| |
1998 |
ID #35597 |
$64,673 |
| |
1999 |
ID #36684 |
$347,365 |
| |
2001 |
|
$749,969 |
(see also: March,
2002 -- AARP Andrus grant for National Quality Partnership
Program) |
| 1999 |
|
Pain Relief Promotion
Act of 1999 (HR 2260; S 1272) AAHPM and Partnership
for Caring opposed the legislation, alleging that it would
have a chilling effect on physicians' prescribing opioids
in sufficient dosage to alleviate pain. |
| 1999 |
|
 “Roman
Catholic EPEC” “Roman
Catholic EPEC”
In 1999, Myles Sheehan, S.J., MD, was awarded a Soros PDIA
grant to create EPEC for Catholics:
"Catholic hospitals are one
of the major providers of healthcare in the United
States. This project focuses on improving care of
the dying through an educational program, at the community
level, for parishes and physicians. The curriculum
will discuss the Catholic tradition of death and dying,
respect for human dignity, pain & symptom relief,
and recognizing the inevitability of natural death."
Sheehan worked with Supportive Care
of the Dying and Partnership for Caring. The result
was unveiled in 2002 in “Recovering
Our Traditions.”
|
| 1999 |
Mar |
 Medical
Textbook Revision. Karen Kaplan of Choice in Dying/Partnership
for Caring later listed what she and Last Acts considered
to be the best medical texts
on end-of-life care. Medical
Textbook Revision. Karen Kaplan of Choice in Dying/Partnership
for Caring later listed what she and Last Acts considered
to be the best medical texts
on end-of-life care. |
| 1999 |
May |
 Meeting
the Challenge: Twelve
Recommendations for Improving End-of-Life Care in Managed
Care is officially released at a National Press
Club conference in Washington, DC. Five managed
care organizations endorsed the study's recommendations:
Aetna/US Healthcare, Allina Health System, Fallon Health
Care Plan, Harvard Pilgrim Healthcare, and HealthPartners.
(Funded by RWJF; conducted by CAEPP at EDC.) Meeting
the Challenge: Twelve
Recommendations for Improving End-of-Life Care in Managed
Care is officially released at a National Press
Club conference in Washington, DC. Five managed
care organizations endorsed the study's recommendations:
Aetna/US Healthcare, Allina Health System, Fallon Health
Care Plan, Harvard Pilgrim Healthcare, and HealthPartners.
(Funded by RWJF; conducted by CAEPP at EDC.) |
| 2000 |
|
National Hospice Organization
reorganizes to form National Hospice and Palliative
Care Organization (NHPCO). |
| 2000 |
|
 National
Hospice Work Group, collaborating with National Hospice
and Palliative Care Organization (NHPCO) launches project:
"Increasing Access to
Hospice." The project is funded in part through
a $125,000 grant from the Nathan Cummings Foundation to
the Hastings Center, awarded in 2000. The study
led to the 2003 publication of "Access
to Hospice Care: Expanding Boundaries, Overcoming
Barriers" (588Kb PDF) as an insert in the Hastings
Center Report National
Hospice Work Group, collaborating with National Hospice
and Palliative Care Organization (NHPCO) launches project:
"Increasing Access to
Hospice." The project is funded in part through
a $125,000 grant from the Nathan Cummings Foundation to
the Hastings Center, awarded in 2000. The study
led to the 2003 publication of "Access
to Hospice Care: Expanding Boundaries, Overcoming
Barriers" (588Kb PDF) as an insert in the Hastings
Center Report |
| 2000 |
|
 Choice
in Dying begins formal reorganization, to become Partnership for Caring. Choice
in Dying begins formal reorganization, to become Partnership for Caring. |
| 2000 |
Jan |
VITAS founder Hugh Westbrook (Florida resident) arranges
a $13.5 million gift to found Duke University Institute
on Care at the End of Life. Three years later,
Westbrook and his wife Carole Shields (People for the
American Way) contribute an additional $3 million. By
2004, Soros/Kornfeld/RWJF grantee Richard Payne, MD,
would be the Institute's director.
[Next: EPEC2] |
| 2000 |
Feb |
 ELNEC
(End-of-Life Nursing Education Consortium) is launched, following research that began with a textbook
study in 1997. ELNEC is end-of-life education for nurses,
similar to EPEC (EOL education for physicians). ELNEC
uses a "train-the-trainer" model. ELNEC
(End-of-Life Nursing Education Consortium) is launched, following research that began with a textbook
study in 1997. ELNEC is end-of-life education for nurses,
similar to EPEC (EOL education for physicians). ELNEC
uses a "train-the-trainer" model.
Funding from RWJF to American Assn.
of Colleges of Nursing (AACN): $3,337,195
- 1997 -- $35,712; Strategy meeting on nursing education
to improve EOL care (#31451)
- 1997 -- $27,116; ELNEC--Strategy meeting (G. Bednash)
- 2000 -- $846,999; ELNEC support (#40766; Ann Rhome)
- 2000 -- $2,224,543; Nursing faculty development
in EOL care (#37617; G. Bednash)
- 2002 -- $202,825; Evaluation of nursing faculty
development in EOL care (A. Rhome)
|
| 2000 |
Mar |
March 7: Byock &
Quill: "Responding to Intractable Terminal Suffering" |
| 2000 |
Apr |
Schiavo:
Terri is moved from nursing home to Hospice of Florida
Suncoast facility. |
| 2000 |
Apr |
 April
20: RWJF awarded $4.7
million to Diane Meier and Christine Cassel to establish Center
to Advance Palliative Care (CAPC) at Mount
Sinai School of Medicine in New York City. The Center,
working with the American Hospital Assn. and EPEC at
the AMA, will develop tools and standards to promote
palliative care in hospitals. (Grant
#37515, 1999). Cassel and Meier were known for their
several articles, written with Timothy Quill, in support
of assisted suicide. April
20: RWJF awarded $4.7
million to Diane Meier and Christine Cassel to establish Center
to Advance Palliative Care (CAPC) at Mount
Sinai School of Medicine in New York City. The Center,
working with the American Hospital Assn. and EPEC at
the AMA, will develop tools and standards to promote
palliative care in hospitals. (Grant
#37515, 1999). Cassel and Meier were known for their
several articles, written with Timothy Quill, in support
of assisted suicide.
Related funding from RWJF:
1999 ID #37515 Mount Sinai School of Medicine -
CAPC $4,742,893
2001 ID #41465 California Health Foundation and Trust
$50,000
2001 ID #41466 Maine Hospital Association, Inc. $50,000
2001 ID #41844 Mount Sinai School of Medicine - CAPC
$36,618
2001 ID #43121 San Diego Hospice $86,400
2001 ID #41464 West Virginia University Foundation,
Inc. $50,000
2001 ID #43952 Mount Sinai School of Medicine - CAPC
$661,040
2002 ID #46432 Bard Group, LLC $225,545
2002 ID #46285 Sutton Group, LLC $400,150
|
| 2000 |
Jun |
 June
5-6: RWJF awards $100,000 to Marian
Gray Secundy, PhD, at Tuskegee University's Center
for Bioethics in Research and Health Care, to host a Roundtable Discussion on African-American Perspectives on End-of-Life Care. The forum commissioned nine papers that "would serve
as the framework for a future national conference." On
2/27/01, ten of the participants met to finalize plans
for the national conference ("Last
Miles" — held in Atlanta in February, 2004).
Marian Gray Secundy had suffered a stroke in 2000. She
left Tuskegee and moved to Washington, DC. in mid-2002.
On December
17, 2002 she died of a heart attack while visiting
her daughter in New York. Subsequent grants for the work
went to Richard Payne, MD, at North General Hospital in
New York, and it would be Dr. Payne and his organization
— IIPCA — that would host "Last Miles."
[Next: EPEC2] June
5-6: RWJF awards $100,000 to Marian
Gray Secundy, PhD, at Tuskegee University's Center
for Bioethics in Research and Health Care, to host a Roundtable Discussion on African-American Perspectives on End-of-Life Care. The forum commissioned nine papers that "would serve
as the framework for a future national conference." On
2/27/01, ten of the participants met to finalize plans
for the national conference ("Last
Miles" — held in Atlanta in February, 2004).
Marian Gray Secundy had suffered a stroke in 2000. She
left Tuskegee and moved to Washington, DC. in mid-2002.
On December
17, 2002 she died of a heart attack while visiting
her daughter in New York. Subsequent grants for the work
went to Richard Payne, MD, at North General Hospital in
New York, and it would be Dr. Payne and his organization
— IIPCA — that would host "Last Miles."
[Next: EPEC2] |
| 2000 |
Jun |
Shift in priorities:
away from "individual choice"
Joanne Lynn, Hal R. Arkes*, et al.: Rethinking
Fundamental Assumptions: SUPPORT's
Implications for Future Reform.
The second phase of SUPPORT had failed. Last
Acts noted in 1996:
"A second phase of [SUPPORT]
revealed even more disturbing findings. The
researchers designed a special intervention using
nurses to facilitate communication between patients
and health care professionals, provide more accurate
assessments of how long a terminally ill patient might
live, and provide the patient and family with a
means of expressing their wishes regarding treatment--including
pain control and heroic measures such as resuscitation.
Despite the diligence of the nurses and other members
of the health care team, the intervention failed to
change the circumstances of death. For example,
the amount of time patients spent in the intensive
care unit before dying was unchanged, and reports
of pain did not decrease. About a third of the
families lost most or all of their savings caring
for the patient."
In Rethinking
Fundamental Assumptions, Dr. Lynn et al. conclude
that better communications (advance directives) and
personal choice will not improve death in America; the
entire medical system and popular culture should be
reformed, creating "a default glide path" for the dying
patient. J Am Geriatr Soc 48:S214-S221, 2000
*(not to be confused with Hadley
Arkes of Amherst) |
| 2000 |
Jul |
Callahan: "Rationing,
Equity, and Affordable Care" (Health
Progress magazine)
|
| 2000 |
Aug |
 Partnership
for Caring is named National Program Office
for Last Acts Partnership
for Caring is named National Program Office
for Last Acts |
| 2000 |
Sep |
 September: Bill Moyers' On
Our Own Terms airs on public television. $2.7
million from RWJF for the $6.25 million production. September: Bill Moyers' On
Our Own Terms airs on public television. $2.7
million from RWJF for the $6.25 million production.
In addition to the television broadcast, On
Our Own Terms featured a local activism
component. Moyers provided coalition leaders
with outreach
materials such as press releases and instructions
on hosting meetings to discuss the broadcast. And during
the broadcast, viewers were encouraged to call in for
information, and to join local
coalitions and national
agencies that had collaborated in the broadcast
production. Compassion in Dying, an organization that
promotes assisted-suicide, provided
volunteers to answer some of the phone lines.
The local activism component — the coalitions
— would provide the framework for Last Acts' Rallying Points (see
below). Rallying Points would launch a
few months later, in January, 2001.
 Prior
to broadcast, Partnership for Caring hosted a Capitol
Hill reception featuring Sen. John D. Rockefeller
(D-WV), Sen. Susan Collins (R-ME), Sen. Ron Wyden (D-OR),
Rep. Jan Schakowsky (D-IL), James Oberstar (D-MN), Frances
Glendening (First Lady of Maryland), Juan Williams,
Daniel Tobin, MD, Joanne Lynn, MD, and Marian Gray Secundy.
(See page 3 of PfC's newsletter Voices, Winter, 2000 for a report with photos; also Americans
for Better Care of the Dying website.) Prior
to broadcast, Partnership for Caring hosted a Capitol
Hill reception featuring Sen. John D. Rockefeller
(D-WV), Sen. Susan Collins (R-ME), Sen. Ron Wyden (D-OR),
Rep. Jan Schakowsky (D-IL), James Oberstar (D-MN), Frances
Glendening (First Lady of Maryland), Juan Williams,
Daniel Tobin, MD, Joanne Lynn, MD, and Marian Gray Secundy.
(See page 3 of PfC's newsletter Voices, Winter, 2000 for a report with photos; also Americans
for Better Care of the Dying website.)
Funding included:
From Nathan Cummings Foundation, Inc.
1997 Educational Broadcasting Corporation $40,000
1998 Educational Broadcasting Corporation $500,000
From Robert Wood Johnson Foundation:
1999 ID #35477 $2,750,000 (Last Acts
site listed grantee
as Public Affairs Television, Inc; RWJF
Annual Report indicates grantee was Educational Broadcasting
Corp.)
2000 ID #38964 American Association of Retired Persons
(AARP) $560,000 (for a special
companion piece in Modern
Maturity. The title of the lead piece
was "The
Last Taboo.")
[Next: First Rallying
Points conference (Jan 2001)]
|
| 2001 |
Jan |
  Karen
Orloff Kaplan of Partnership for Caring calls the first Rallying Points meeting
in Newport Beach, California, on January 8. This first
conference is a gathering of about 300 people from
across the US who participated in Bill Moyers' On
Our Own Terms program. Rallying Points would
not be formally launched until the next year (see February, 2002). Its
purpose is "a
bottom-up approach to changing the attitudes towards
death and dying of consumers, providers and health care
institutions. It is intended to complement the top-down
strategies of Last Acts and other organizations that
work at the national level to change the public mindset
. . . " Karen
Orloff Kaplan of Partnership for Caring calls the first Rallying Points meeting
in Newport Beach, California, on January 8. This first
conference is a gathering of about 300 people from
across the US who participated in Bill Moyers' On
Our Own Terms program. Rallying Points would
not be formally launched until the next year (see February, 2002). Its
purpose is "a
bottom-up approach to changing the attitudes towards
death and dying of consumers, providers and health care
institutions. It is intended to complement the top-down
strategies of Last Acts and other organizations that
work at the national level to change the public mindset
. . . "
[Next: RP resource centers (Feb 2002) ] |
| 2001 |
Feb |
 Faith
in Action national program office moves to Wake
Forest University School of Medicine in North Carolina.
The RWJF
grant report notes: "This $100-million expansion
is a seven-year initiative . . . that is supporting
the start-up of up to 2,000 new Faith in Action coalitions,
with special consideration to programs that are designed
to reach low-income or underserved communities.
Faith in Action, Generation 3 will try to reach these
groups through organizations that are connected to them,
such as the National Council of La Raza, which represents
Latinos; the Islamic Society of North America, which
represents Muslims; African-American congregations;
and groups that work in rural areas. These organizations
may help Faith in Action, Generation 3 identify sites
that it might not learn about on its own." The
program office at Wake Forest received over $15 million
from RWJF from 2001-2004, which did not include the
grants to coalitions, each of which were about $35,000. Faith
in Action national program office moves to Wake
Forest University School of Medicine in North Carolina.
The RWJF
grant report notes: "This $100-million expansion
is a seven-year initiative . . . that is supporting
the start-up of up to 2,000 new Faith in Action coalitions,
with special consideration to programs that are designed
to reach low-income or underserved communities.
Faith in Action, Generation 3 will try to reach these
groups through organizations that are connected to them,
such as the National Council of La Raza, which represents
Latinos; the Islamic Society of North America, which
represents Muslims; African-American congregations;
and groups that work in rural areas. These organizations
may help Faith in Action, Generation 3 identify sites
that it might not learn about on its own." The
program office at Wake Forest received over $15 million
from RWJF from 2001-2004, which did not include the
grants to coalitions, each of which were about $35,000.
In October, the Family Caregiver Alliance
will host a conference
To see lists of coalitions by state,
visit the Faith
in Action website. Here is a sample
list of Faith in Action
grants, circa 2002-2003.
|
| 2001 |
Jun |
 California:
In Bergman v. Chin,
jury finds Dr. Chin guilty of negligence in under-prescribing
pain medication, and awards $1.5 million to Bergman. California:
In Bergman v. Chin,
jury finds Dr. Chin guilty of negligence in under-prescribing
pain medication, and awards $1.5 million to Bergman.
|
| 2001 |
Sep |
 Finding
Our Way: Living With Dying in America Finding
Our Way: Living With Dying in America
A 15-part newspaper series carried
by Knight-Ridder, meant to build on Moyers' television
series. As Partnership for Caring wrote in their newsletter,
"Building on the momentum of the highly successful community
outreach associated with last year’s PBS airing
of On Our Own Terms, Moyers On Dying which had
an audience nearly 60% larger than the PBS prime-time
average the local coalitions hope to stimulate a similar
response with Finding Our Way."
Funding for Finding
Our Way: $300,000 from RWJF to Daniel Tobin's
"Life Institute;" and $150,000 from Samuels Foundation
to Partnership for Caring.
Though the program had been planned
long before September 11, Last Acts released the new
program as part of a grief management program in response
to the World Trade Center attack, with the headline
"Nation's Largest Health Foundation Commits Multi-Million-Dollar Response
to Terrorism."
|
| 2001 |
Oct |
In conjunction with Compassion in Dying's case Bergman
v. Chin, the California legislature passes Assembly
Bill 487. Last Acts cites the legislation
as an exemplary state initiative in their November,
2002, report Means
to a Better End:
"This case inspired the
California legislature to pass Assembly Bill 487,
signed into law October 4, 2001. The new law requires
that physicians who
fail to prescribe, administer or dispense adequate
pain medication be charged with unprofessional conduct
and be investigated by the California Medical Board’s
Division of Licensing. Physicians found guilty of
undertreating pain must complete a pain-management
education program."
|
| 2001 |
Oct |
   Last
Acts enlists Hollywood: Last
Acts enlists Hollywood:
Seminar hosted by the Last
Acts Writers Project, October 17, 2001, brought
Compassion in Dying together with Last Acts to coach
television and movie writers on end-of-life scripts.
Subjects covered included the Wendland case, and Bergman
v. Chin. Panelists included
- Nancy N. Dubler, author and director, Division of
Law and Ethics, Montefiore Medical Center, Bronx,
NY; member of the American Bar Association's Commission
of Legal Problems of the Elderly.
- Vicki Michel, co-chair, Los Angeles Bar Association/Medical
Association Joint Committee on Biomedical Ethics;
authored amicus brief in the Wendland right-to-die
case (in favor of removing Robert Wendland's food
& hydration(
- Michael Gilfix, Gilfix & LaPoll, Palo Alto,
California (Partnership for Caring)
- James Geagan, lead trial counsel in Bergman
v. Chin, represented the Compassion in Dying
Federation.
- Moderator: Terrance A Sweeney, vice-president of
Paulist Productions; moderator of Humanitas Master
Writers Workshops in Los Angeles.
Co-Sponsors: The American Bar
Association; The End of Life Work Group of the National
Association of Attorneys General; Freelance Committee
of the Writers Guild; Los Angeles County Medical Association/Bar
Association Joint Committee on Biomedical Ethics; Partnership
for Caring and the Compassion in Dying Federation.
In 2002, Not Dead Yet remarked on the
bias in this conference, noting that the Wendland case was discussed extensively, but only the
losing side (Compassion in Dying et al.) was represented.
Principals of Not Dead Yet were knowledgeable in the
case, having filed an amicus brief in support of allowing
Robert Wendland to live. Not Dead Yet would also
object to Last Acts' portrayal of Michael J. Fox as
a dying man, rather than as a person living with Parkinson's.
(Moving death-acceptance upstream,
to the moment of diagnosis, is arguably part of the
process of moving palliative care and hospice upstream.
Michael J. Fox's description of himself as a dying man
so early in the course of his illness demonstrates the
sad outcome of such a plan.)
Partnership for Caring's Fall,
2001, newsletter claimed "story lines on ER, NYPD Blue, Gideon’s Crossing and City of Angels [also Touched by an
Angel, Law
& Order, and CSI],
can be attributed to the Writers Project." Noah
Wyle of ER would become spokesperson for RWJF's "Cover the Uninsured
Week" in addition to promoting the Last Acts message.
|
| 2001 |
Oct |
October 26-27:
Family Caregiver Alliance, funded by RWJF, hosts national
conference for state policy-makers, and provides technical
assistance to Hillary Clinton to produce the Lifespan
Respite Care Act. (RWJF
grant #40402; $231,530). |
| 2001 |
Dec |
December 5; Washington, DC. Alliance
for Health Reform (AHR) hosts a briefing
titled "Approaching Dying: Improving How We Pay
for Care Near the End of Life." Paid
for by RWJF. (The RWJF 2001 Annual Report shows they
gave $1.5 million to AHR over 3 years). There
is no indication as to how many journalists or legislators
attended the brown-bag lunch, but the online transcript includes Karen Kaplan's abbreviated summary of Last
Acts and description of "the gold standard" in end of
life care. Also in the transcript is Edward
Howard (AHR) relating an early connection between
Alliance for Health Reform and Karen Kaplan:
"Karen Kaplan . . . is President
and CEO of the Partnership for Caring which is an
organization with roots that go back more than, what,
half a century in helping those approaching death
and their families. . . . She founded and ran the
Center for Social Policy and Practice at the National
Association for Social Workers where, as I was telling
Don [Schumacher], she served as sort of the business
incubator, if you will, of the Alliance for Health
Reform a number of years ago."
(AHR Chair and Vice-Chair are Senators Jay Rockefeller
and Bill Frist).
|
| 2001 |
|
 December
12: National
Consensus Project is launched at a leadership meeting in New York
City. (This is a Partnership for Caring project; convened
by Diane Meier). Goal: "to arrive at a mutually agreed
upon definition of palliative care and identify the
standards and guidelines necessary for the practice
of high quality palliative care." December
12: National
Consensus Project is launched at a leadership meeting in New York
City. (This is a Partnership for Caring project; convened
by Diane Meier). Goal: "to arrive at a mutually agreed
upon definition of palliative care and identify the
standards and guidelines necessary for the practice
of high quality palliative care."
Collaborating to produce
the consensus statement:
American Academy of Hospice and Palliative
Medicine (AAHPM);
Center to Advance Palliative Care (CAPC);
Hospice and Palliative Nurses Association
(HPNA);
National Hospice and Palliative Care Organization
(NHPCO);
Partnership for Caring (PfC).
 Steering
committee includes: Diane Meier, Betty Ferrell, Robert
Arnold, Andrew Billings, Mary Labyak, Charles von Gunten,
Judith Peres, True Ryndes, Russell Portenoy. Steering
committee includes: Diane Meier, Betty Ferrell, Robert
Arnold, Andrew Billings, Mary Labyak, Charles von Gunten,
Judith Peres, True Ryndes, Russell Portenoy.
In 2004, the group produces the first
consensus document. (see Clinical
Practice Guidelines for Palliative Care, April,
2004)
|
| 2002 |
|
 RWJF
awards Richard
Payne, MD, and North General Hospital in New York,
$446,990 (grant #43073) for
"the EPEC2 Project: End-of-life
care education for African-American health care professionals."
This later became known as the "APPEAL
Project." Meanwhile, Project on Death in America awards
Payne $166,224 to create the Initiative to Improve
Palliative Care for African-Americans (IIPCA). RWJF
awards Richard
Payne, MD, and North General Hospital in New York,
$446,990 (grant #43073) for
"the EPEC2 Project: End-of-life
care education for African-American health care professionals."
This later became known as the "APPEAL
Project." Meanwhile, Project on Death in America awards
Payne $166,224 to create the Initiative to Improve
Palliative Care for African-Americans (IIPCA).
IIPCA aims to eliminate racial disparities in access to end-of-life
care. The question becomes, "what is optimum care?"
In 2001, Dr. Payne reported on the disparate
views between African-American physicians and
white physicians. The Last Acts movement had been
built on inferences from the SUPPORT study: that
patients do not want (and should not request) life-prolonging
procedures. African-American physicians, it seems,
were 180-degrees off of the Last Acts course.
Dr. Payne wrote (emphasis added):
"There appear to be significant
differences in attitudes between African-American
and white physicians about care at the end of their
patients’ lives and their own (Mebane et al.,
1999). For example, white
physicians more often view tube feedings as “heroic”
measures in terminally ill patients than do
African-American physicians (58 percent vs. 25 percent).
In this same study, 36 percent of white physicians
accept physician-assisted suicide (PAS) as a treatment
alternative, while only 26.5 percent of African-American
physicians do. When asked about care for themselves
at the end of life, this study also observed startling differences between white and black physicians. For
example, if in PVS,
African-American physicians were six times more likely
than whites to request aggressive treatment.
In a scenario in which the doctors might be brain
damaged but not terminally ill, the majority of both
groups did not want aggressive treatment, but African-American
physicians were five times more likely than whites
to request specific aggressive treatment (23
percent vs 5 percent) and white physicians were two
times more likely to request PAS than African Americans
(22.5 percent vs. 9 percent). "
[Institute of Medicine.
National Research Council. In: Improving Palliative
Care for Cancer. National Academy Press.
Washington DC, Foley & Gelband, p156, 2001.] |
| 2002 |
Jan |
January 3-4: Funded
in part by $75,000 from Project on Death in America, Richard
Payne and IIPCA host their first conference, "Heritage,
Health, and Hope," moderated by Juan Williams. |
| 2002 |
Feb |
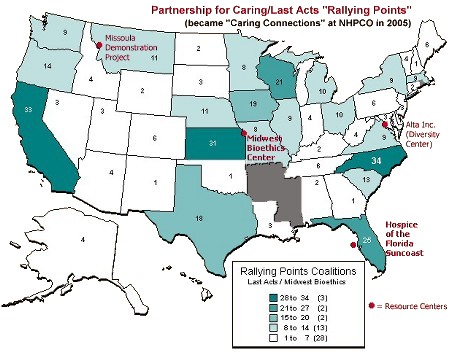
  February: Last Acts formally announces the Rallying
Points project. Four months prior, RWJF
awarded $12 million to Karen Orloff Kaplan and Partnership
for Caring (director of Last Acts) to establish Rallying
Points and build upon the 300+ grass roots coalitions
established by Bill Moyers' public television broadcast On Our Own Terms.
February: Last Acts formally announces the Rallying
Points project. Four months prior, RWJF
awarded $12 million to Karen Orloff Kaplan and Partnership
for Caring (director of Last Acts) to establish Rallying
Points and build upon the 300+ grass roots coalitions
established by Bill Moyers' public television broadcast On Our Own Terms.
| Click here for
larger map. |
| Click red Resource Center names to
view their funding. |
|
Partnership for Caring named four resource
centers that would counsel the coalitions. Three of
the centers were regional centers as well as specialists
in a field of concern to the activists:
- Midwest Bioethics Center a/k/a
Center for Practical Bioethics (Midwest region; specializing
in advance directives; home of "Community-State Partnerships");
- Hospice
of the Florida Suncoast (Eastern region;
specializing in community-level public education);
[see below: Terri
Schiavo]
- Ira Byock's Missoula Demonstration Project (Western region; specializing in community-based research
and developing needs assessments)
and the National
Resource Center on Diversity in End-of-Life Care,
directed by Alta Consulting Group, in Washington,
DC, was named as a resource to promote culturally sensitive
end-of-life care in minority communities.
That year (2002) Partnership for Caring paid to:
- Midwest Bioethics Center: $301,200
- Hospice of the Florida Suncoast: $300,000
- Life's End Institute (Missoula): $300,000
- Alta Consulting: $300,000
- Stewart Communications (social marketing firm):
$376,732
Sample activities:
- Hospice
of the Florida Suncoast provides ELNEC training
for Carolinas hospice nurses (annually).
- Through Midwest Bioethics, Rallying
Points announces (August 2003): "The Carolinas
Center for Hospice & End of Life Care (NC &
SC) will present an "Advance Care Planning Summit:
Bringing Vision into Focus" featuring William Colby,
JD, author of Long Goodbye: The Deaths of Nancy Cruzan"
- The resource centers create guides on how to start
a coalition, how to host town hall meetings, diversity
in EOL care -- at the Carolinas
Center web site.
- Coalitions were encouraged to use the online "Community
Tool Box" provided by the University of Kansas.
For an example of the tools offered, explore Chapter
30: "Principles
of Advocacy" ("Identifying Opponents," and "Encouraging
Involvement of Potential Opponents."). Chapter 35
features an "Overview of Opposition Tactics."
[ Next: Partnership
for Caring, right-to-die and euthanasia advocate group
that directed Rallying Points, transforms again into "Last
Acts Partnership," and receives another large
grant.] |
| 2002 |
Feb |
February 12: Minimally Conscious State (MCS): definitions
and diagnostic criteria Neurology. 2002 Feb 12;58(3):349-53.
Developed from meetings of the Aspen Neurobehavioral
Conference Workgroup.
Authors: Joseph T. Giacino, PhD; Stephen Ashwal,
MD; Nancy Childs, MD; Ronald Cranford, MD; Bryan Jennett,
CBE, MD, FRCS; Douglas I. Katz, MD; James P. Kelly,
MD; Jay H. Rosenberg, MD; John Whyte, MD, PhD; Ross
Zafonte, DO. |
| 2002 |
Mar |
NHPCO receives $100,000
grant from AARP Andrus Foundation for NHPCO's National
Quality Partnership Program. Objective of the
program is:
"to develop performance measures derived from the following
primary goals – or outcomes – of hospice
and palliative care:"
- Comfortable Dying,
- Safe Dying,
- Self Determined Life Closure [?]
- Effective Grieving.
|
| 2002 |
Jun |
 Compassion
in Dying's pain control case -- Bergman
v. Chin -- is settled by an Alameda County,
CA, judge. Dr. Chin is required to pay 150% of the
Bergman's attorney fees (James Geagan, the lead attorney,
was a Compassion in Dying cooperating attorney). Compassion
in Dying's pain control case -- Bergman
v. Chin -- is settled by an Alameda County,
CA, judge. Dr. Chin is required to pay 150% of the
Bergman's attorney fees (James Geagan, the lead attorney,
was a Compassion in Dying cooperating attorney). |
| 2002 |
Jun |
Rosalynn Carter (honorary
chair of Last Acts) and Hillary Clinton are the featured
speakers at the Family
Caregiving Conference held by the National Health
Council and National Quality Caregiving Coalition. Press
release gives a nod to Lifespan Respite Care Act which
Sen. Clinton had introduced the previous month; as well
as to RWJF's $100 million commitment to Faith in Action. |
| 2002 |
Sep |
National
Association of Attorneys General (NAAG) president Drew Edmondson (Oklahoma) hosts the first of
three "listening conferences" as part of a NAAG Presidential
Initiative to promote state advance directive reforms
and state pain initiatives. |
| 2002 |
Nov |
 November:
RWJF's Means
to a Better End: A Report on Dying in America Today.
November 18th press
conference announcing the results features James
Towey, Drew Edmondson (National Association of Attorneys
General), and Judith Peres of Partnership for Caring/Last
Acts. RWJF's quarterly newsletter Advances featured a summary of the project. (The newsletter
also interviews PfC's Judith Peres, and provides several
revealing comments. One example, particularly ironic
in light of the Schiavo case: "In one study, 55 to 75
percent of people in the ICU said that they were hungry
and thirsty, and in moderate to severe pain. That's
not how people want to die.") November:
RWJF's Means
to a Better End: A Report on Dying in America Today.
November 18th press
conference announcing the results features James
Towey, Drew Edmondson (National Association of Attorneys
General), and Judith Peres of Partnership for Caring/Last
Acts. RWJF's quarterly newsletter Advances featured a summary of the project. (The newsletter
also interviews PfC's Judith Peres, and provides several
revealing comments. One example, particularly ironic
in light of the Schiavo case: "In one study, 55 to 75
percent of people in the ICU said that they were hungry
and thirsty, and in moderate to severe pain. That's
not how people want to die.")
Last Acts provided public
relations information to state coalitions.
For example, a press
release was provided for distribution by the Maine
Hospice Council.
Be sure to visit the interactive map
of the US [click here,
then click on the first item, "Means to a Better End"]
showing which states meet their standards. For example,
the map shows that based on an American Bar Association
assessment, Florida merits an "A" for its advance directives
laws.
|
| 2003 |
Feb |
 Last
Acts Palliative Care Committee produces "On the Road from
Theory to Practice" Last
Acts Palliative Care Committee produces "On the Road from
Theory to Practice" |
| 2003 |
Feb |
Cassel & Quill "Position Paper" on Assisted Suicide.
They recommend that medical groups do not take a position
on PAS. Instead, they urge a position of "studied neutrality."
Annals
of Internal Medicine.
Vol. 138, Issue 3, pp. 208-211. |
| 2003 |
Mar |
AARP's Modern Maturity magazine publishes article supporting assisted-suicide.
|
| 2003 |
Apr |
NHPCO hosts a Research
Conclave of about 30 leading palliative care experts.
A press
release states: "One of the primary
purposes of the conclave was to identify priorities
for research funding that NHPCO can support. NHPCO intends
to advocate with Congress, the National Institutes of
Health, the Veterans Administration, and with private
foundations and individuals interested in supporting
research to advance the field." [An 85-page
transcript of the meeting is available online.]
Donald Schumacher remarked:
"NHPCO
is about ready to change its face pretty dramatically
over the next couple of months and then through the
next year. One of our initiatives in addition to finding,
moving into a building that would be in Washington,
focusing in on end of life care, global leadership
center - an opportunity for us to expand the care
that we’ve been doing at end of life to other
areas of the field, such as focusing in on care for
with persons with HIV and AIDS; and also diversity,
care for children and adolescents, section on spirituality…"
Christina Puchalski (Last Acts Spirituality Task Force
convener), noted:
"we’re really pretty brand
new with [developing tools to measure] spirituality
even though there’s thousands of years of thought
and literature behind it. What we need to do is to
translate that and some of us are trying to do that,
that thousands of years of thought into measures we
might use, for example, in end of life research. So
someone may be in spiritual distress, but that’s
not necessarily spiritual unhealthiness, it might
be spiritual health - so we have to just keep that
in mind, that differentiation."
Participants included (in alphabetical order):
- Kimberly Acquaviva, Ph.D., MSW (Hospice of
Florida Suncoast);
- Susan Block, M.D. (PDIA);
- Ira Byock, M.D.;
- David Casarett, M.D., M.A (Greenwall, Commonwealth
Fund, NIH);
- Stephen Connor, Ph.D. (PDIA, AARP, RWJF);
- Kathleen (Kathy) Egan, MA, BSN (Hospice of
Florida Suncoast, NIH);
- Perry Fine, M.D. (Partnership for Caring;
VistaCare);
- John Finn, M.D. (AAHPM, Hospice of Michigan);
- Kathleen Foley, M.D. (PDIA);
- Joanne Hilden, M.D. (PDIA; Cleveland Clinic);
- Rabbi Barry Kinzbrunner, MD (VITAS; AAHPM);
- Jean Kutner, M.D. (PoPCRN; Univ. of Colorado;
RWJF);
|
- Gwendolyn London, D.Min.;
- Joanne Lynn, M.D., MA, MS;
- Neil MacDonald, CM, MD;
- Melanie Merriman, Ph.D., M.B.A.;
- Frederick Meyers, M.D;
- Robert Milch, M.D.;
- Susan Miller, Ph.D., MBA;
- Sean Morrison, M.D.;
- J. Cameron Muir, M.D., FAAHPM;
- Steven Passik, Ph.D.;
- Elizabeth Pitorak, MSN, RN, CHPN (RWJF; Hospice
of the Western Reserve);
- Christina Puchalski, M.D. (RWJF);
- True Ryndes, ANP, MPH (Partnership for Caring;
RWJF);
- Donald Schumacher, Psy.D (Partnership for
Caring; RWJF);
- Karen Steinhauser, Ph.D.;
- Patti Thielemann, PhD;
- Diana Wilkie, Ph.D., R.N.
|
|
| 2003 |
Apr |
Chair of the Palliative
Medicine Review Committee (PMRC), Steven Radwany,
MD, travels
to Cuba. PMRC is a joint effort of American Academy
of Hospice and Palliative Medicine (AAHPM) and
the American Board of Hospice and Palliative Medicine
(ABHPM), and was formed to accredit palliative
medicine residency programs. |
| 2003 |
May |
 May
15: National Association of Attorneys General
(NAAG) Listening
Conference Improving End-of-Life Care (Midwest Bioethics,
PfC, RWJF) May
15: National Association of Attorneys General
(NAAG) Listening
Conference Improving End-of-Life Care (Midwest Bioethics,
PfC, RWJF) |
| 2003 |
Jul |
Edward Yellig, MD, medical
director of Hospice of Wake County, North Carolina, writes
an article titled "Palliative Sedation" which is published
in the Wake County Physician, the newsletter
of the Wake County Medical Society (Summer--3rd
Quarter, 2003). The article was a case study
on the use of terminal sedation, coupled with withdrawal
of food and fluids, to end the life of a 68-year old tobacco
farmer who was suffering from dementia. |
| 2003 |
Jul |
PDIA and Kornfeld Foundation collaborate on a palliative care fellowship program
to train physicians in palliative care, and to establish
palliative care as a recognized sub-specialty.
$1.9 million would fund 13 programs:
Round One (2003-2005):
- The Palliative Care Program at Marshfield Clinic,
Marshfield, WI; Michael Claessens, M.D.
- The Hospice/Palliative Training Program at the University
of New Mexico Health Sciences Center, Albuquerque,
NM; Walter Forman, M.D.
- Combined Fellowship in Pediatric & Adult Palliative
Medicine at the Medical College of Wisconsin Affiliated
Hospitals, Milwaukee, WI; Bruce Himelstein, M.D.
- The Pain and Palliative Care Service in the Department
of Neurology of Memorial Sloan-Kettering Cancer Center,
New York, NY; Richard Payne, M.D.
- Center for Palliative Studies at San Diego Hospice,
San Diego, CA; Charles von Gunten, M.D., Ph.D., FACP
- The Palliative Care and Home Hospice Program at
Northwestern; Memorial Hospital, Chicago, IL; Jamie
von Roenn, M.D.
- Palliative Care Fellowship Program, Section of Palliative
Care and Medical Ethics, University of Pittsburgh,
Pittsburgh, PA; Linda King, M.D.
Round Two (2004-2006):
- The Palliative Care and Home Hospice Program at
Northwestern Memorial Hospital/Feinberg School of
Medicine, Northwestern University, Chicago, IL; Jamie
von Roenn, M.D.
- The George Washington University Palliative Care
Fellowship Program, Washington, D.C.; Elizabeth Cobbs,
M.D.
- Fellowship in Palliative Medicine, Duke University
Medical Center, Durham, NC; James Tulsky, M.D., Anthony
Galanos, M.D.
- Children’s Hospital Boston Pediatric Advanced
Care Team/Dana; Farber Cancer Institute, Boston, MA;
Joanne Wolfe, M.D.
- The Harry R. Horvitz Center for Palliative Medicine/Cleveland;
Clinic Taussig Cancer Center, Cleveland, OH; Susan
LeGrand, M.D.
- Montefiore Medical Center Palliative Care Program/Albert
Einstein; College of Medicine, Bronx, NY; Sean O'Mahony,
M.D.; Peter Selwyn, M.D., M.P.H.
In addition, PDIA announces
that "as part of its exit strategy," it will award AAHPM $1.2 million for the purpose of creating a College
of Palliative Medicine. |
| 2003 |
Jul |
 Hemlock
Society (Denver, CO) changes its name to End
of Life Choices. They launch a new
web site. Hemlock
Society (Denver, CO) changes its name to End
of Life Choices. They launch a new
web site. |
| 2003 |
Aug |
Physicians for
a National Health Program issue call
for universal health care, published in JAMA. Principals
of PNHP include Christine Cassel and Marcia Angell. The
PNHP web site lists endorsers, including: Diane
Meier, Edward Yellig, Robert Truog, James Tulsky, Daniel
Sulmasy. See the Physicians Working Group for Single-Payer National Health Insurance website for
the proposal. |
| 2003 |
Aug |
 RWJF
announces funding available for Palliative
Care Leadership Centers, a $4.5 million program directed
by Diane Meier's Center to Advance Palliative Care (CAPC)
at Mount Sinai in New York. The centers provide
mentoring and site visits for health care professionals
planning a new hospice or hospital palliative care program.
By 2004,
150 healthcare institutions would participate in the
program. RWJF
announces funding available for Palliative
Care Leadership Centers, a $4.5 million program directed
by Diane Meier's Center to Advance Palliative Care (CAPC)
at Mount Sinai in New York. The centers provide
mentoring and site visits for health care professionals
planning a new hospice or hospital palliative care program.
By 2004,
150 healthcare institutions would participate in the
program.
The foundation will award grants to these Palliative
Care Leadership Centers:
- Fairview Foundation (Fairview Health Services)--
Minneapolis, MN
- Massey Cancer Center of Virginia Commonwealth University
Health System-- Richmond, VA
- Medical College of Wisconsin-- Milwaukee, WI
- Mount Carmel Health System-- Columbus, OH
- Palliative Care Center of the Bluegrass-- Lexington,
KY
- University of California, San Francisco-- San Francisco,
CA
|
| 2003 |
Oct |
On October 15, by order
of Pinellas-Pasco Circuit Judge George Greer,
the feeding tube is removed from Terri
Schindler-Schiavo. Terri Schiavo
had been moved from a nursing home to Hospice
House - Woodside, a facility owned and managed
by Hospice
of the Florida Suncoast (a Rallying
Points and Last Acts resource center).
That same day, National Hospice
and Palliative Care Organization (NHPCO) issued
a press
release emphasizing that Hospice House-Woodside
was merely following orders: "Hospice
does not make decisions for patients or families,
nor sit in judgement [sic] of their choices."
The release closes with the comment that
"NHPCO wishes to acknowledge
the quality care being provided and hopes that
the family, caregivers and all those touched by
this tragic situation may find peace and healing
in the days ahead." NHPCO apparently thought
this was end-of-discussion with regard to Terri
Schindler-Schiavo.
Far from ending discussion, the
feeding tube removal brought outspoken criticism
from the public.
While many in
the right-to-die and EOL movement (including bioethicists)
either supported Michael Schiavo or maintained
a position of "studied neutrality," the Terri
Schindler-Schiavo's parents received support from people across the country and around the
world. Medical professionals, talk radio, columnists,
disability activists, and the general public were
horrified that Terri Schiavo would be intentionally
starved and dehydrated to death.
On October 20, five days after
the tube was removed, the Florida legislature
called a special session, and the next day "Terri's
Law" (Florida House Bill 35-E) was passed and
signed by Governor Jeb Bush. This paved
the way for Governor Bush to issue an executive
order to resume Terri's feeding.
On October 29 Michael Schiavo
filed suit against Governor Bush, claiming that
Terri's Law was unconstitutional.
(The Schiavo case involves health care decisions
without a written advance directive. This
is a matter of "health care agency" -- a subject
addressed by the Samuels Foundations' health
care agency initiative centered at Partnership
for Caring.) |
|
| 2003 |
Nov |
November 9: Boston
Globe reports, "After 10 years, $200m
effort on dying reaches its own end" (by
Carey Goldberg, Globe Staff, 11/9/2003)
". . . In particular,
the Project on Death in America, financed by billionaire
George Soros and the Robert Wood Johnson Foundation,
poured more than $200 million over the last decade
into end-of-life programs and research.
But now the Project on Death
is itself dying, and the Robert Wood Johnson Foundation
is phasing out almost all related projects and shifting
toward childhood obesity and the nursing shortage."
|
| 2003 |
Nov |
November: Rallying Points
National convention; Boston. The theme is social
change. |
| 2003 |
Dec |
 Partnership
for Caring hosts a conference call with their
partners, announcing their merger with Last Acts.
They change their name to Last
Acts Partnership. Partnership
for Caring hosts a conference call with their
partners, announcing their merger with Last Acts.
They change their name to Last
Acts Partnership.
[Next: Last
Acts Partnership receives more money. ] |
| |
|
[back] [next]
Updated
on
May 19, 2008 8:23
Unpublished work © Copyright 2004-2008 I. Whitlock. |
|
|
 |